Implanting Microdevices Into Brain Tumors To Determine the Best Treatment
Testing drugs in gliomas prior to systemic treatment could increase chances of success

Complete the form below to unlock access to ALL audio articles.
Malignant brain tumors account for 1–2% of all types of cancers in adults and remain one of the hardest types of cancer to treat. A multi-institutional study published in Science Translational Medicine, led by Dr. Pierpaolo Peruzzi at Brigham and Women’s Hospital, demonstrates the potential for using intratumoral microdevices (IMDs) to test various cancer drugs on the tumor before implementing systemic treatment.
The challenge of heterogeneity in brain tumors
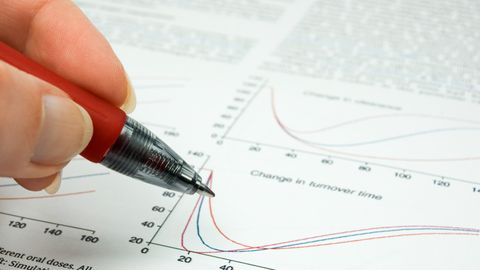
Gliomas, one of the most aggressive forms of brain tumors in humans, have been researched heavily over the past decades and various genes have been implicated in this cancer, including EGFR, PDGFRA, and TP53. Therapies have been developed to target these genes and inhibit cancer growth and proliferation. While these therapies have been successful in preclinical models, many of them have shown variable success in clinical testing, largely because every glioma has a distinct genetic makeup and developing therapies that can target mutant genes in all patients is extremely difficult. Therefore, it has become evident that cancer treatments for patients would be most effective if they are created based on the specific genetic profile of the tumor at hand. Inspired by this era of personalized medicine, Peruzzi et al. developed tiny biocompatible IMDs that can be inserted into the tumor at the time of surgery and release small doses of different drugs at distinct points in the surrounding tissue over the course of two hours. Afterwards, the tissue can be analyzed to measure the impact of each individual drug on the cancer’s growth and proliferation.
Assessing safety and efficacy of microdevices in delivering drugs
Six patients diagnosed with brain tumors were enrolled in the study (50% female, 50% male). The median age of the participants was 76 years, with a range between 27 and 86 years of age. All patients were already scheduled to undergo tumor resection surgery during which each had two IMDs implanted at the tumor site, giving a total of implanted 12 IMDs. The researchers delivered nine drugs through the IMDs, specifically temozolomide, doxorubicin, lapatinib, lomustine, irinotecan, carboplatin, osimertinib, abemaciclib and everolimus. They measured the safety of the IMDs in all patients and analyzed the feasibility of conducting molecular analysis on the tissue after surgery. They assessed DNA damage (via pH2AX expression) and apoptosis (via CC3 expression) in the tissue surrounding the IMD, as well as measuring how distance from the implantation site impacted the degree of drug effect.
The key findings of the paper were:
- The IMD implantation resulted in no adverse events or significant changes in surgical outcomes or cost, and 11 out of the 12 implantations resulted in tissue specimens that could be successfully processed in molecular analysis.
- The greatest degree of DNA damage in the surrounding tissue was found in patient 3, where 65.8% of the cells were impacted, and the lowest amount was found in patient 5, where 9.8% of the cells were impacted.
- Apoptosis induction was generally low (< 5%), except in patient 3, where it was measured in 13.1% of the cells.
- The greatest DNA damage was found in tissue near the IMD site and was found to decrease with lower doses.
- Changes in gene transcription on a drug-to-drug basis correlated with the pathways each drug targeted, confirming that the drugs worked as expected.
Analyzing tissue from the IMD site to determine drug efficacy
Dr. Peruzzi and his team have demonstrated the potential that IMDs have in quickly assessing the best treatment for a specific patient’s brain tumor. The implementation of IMDs was safe in all patients and did not impact the outcomes of surgical procedures or increase surgical costs significantly. By measuring the amount of DNA damage and apoptosis in the tissue surrounding the IMD, the researchers were able to assess the impact that each drug had on cancer progression, as each drug was released in a distinct location within the tissue. A variable range of DNA damage was seen from patient to patient, which could be due to the heterogeneity of tumors. Furthermore, DNA damage appeared to be concentrated at the IMD site, indicating that the delivery of treatment was localized.
While this study displays the promise that IMDs could have in the treatment of brain tumors, there are limitations to the work. Firstly, since the IMD implantation was conducted in patients who were already undergoing scheduled surgery, the IMD could only be inside the tumor for around 2 hours, which may not have been enough time to observe changes in markers for apoptosis. Furthermore, the study consisted of a small population size, and larger clinical studies will need to be conducted to confirm the predictive capability of IMDs.
The need for larger and longer clinical studies
Brain tumors remain one of the hardest cancers to treat, largely due to their heterogeneity, but Peruzzi et al. have developed a viable technology that can provide physicians with information as to what treatments are the most effective for a given patient’s tumor. Larger clinical studies that build upon this research should consider ways to leave the IMD in the tumor for longer periods of time, to maximize the effect that these drugs can have on the surrounding tissue and provide doctors with more accurate information regarding their efficacy. In an era of personalized medicine, IMDs could hold the key for the future of cancer treatment and clinical care.
Reference: Peruzzi P, Dominas C, Fell G, et al. Intratumoral drug-releasing microdevices allow in situ high-throughput pharmaco phenotyping in patients with gliomas. Sci Transl Med. 2023;15(712):eadi0069. doi:10.1126/scitranslmed.adi0069