Four New AML Studies Funded by Leukaemia UK
Even after the grueling ordeal of AML treatment, survival rates from AML are one of the lowest for all forms of cancer.
Complete the form below to unlock access to ALL audio articles.
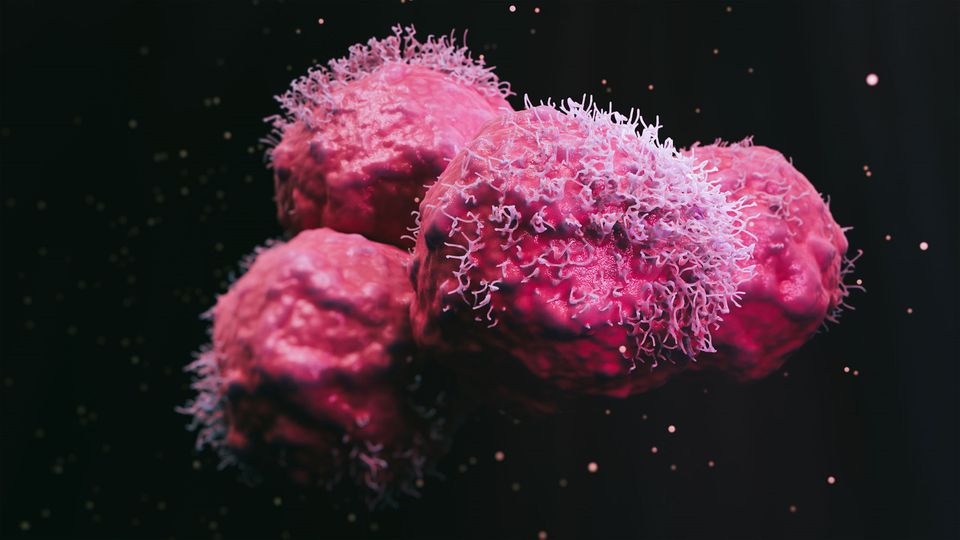
Each year, acute myeloid leukemia (AML) affects over 3,000 people in the UK. Survival rates from AML are estimated at 13.6% after 5 years, one of the lowest rates for all forms of cancer.
Leukaemia UK recently announced that it will channel £600,000 into four new research projects as part of the John Goldman Fellowship scheme. Each project is aimed at finding kinder, more effective treatments for AML. Technology Networks spoke to Kate Nash, research communications manager at Leukaemia UK, to find out more about the current landscape of AML treatment and the innovative research projects aiming to improve the lives of those with the disease.
Kate Robinson (KR): What is the current first line treatment for AML, and are there any challenges associated with AML treatment?
Kate Nash (KN): Chemotherapy is the main treatment utilized for AML. A combination of two or more chemotherapy drugs is normally used. The two main drugs are cytarabine and daunorubicin, but others such as idarubicin, mitoxantrone and etoposide can be used. Other treatments for AML can include radiotherapy or leukapheresis, which removes abnormal white blood cells. The treatment offered will depend on the severity of the white blood cell count, the patient’s age and wellbeing, and the presence of any gene mutations.
Once in remission, further treatment is generally required to prevent the AML from returning. High dose chemotherapy is sometimes followed by a stem cell or bone marrow transplant. A transplant gives patients the best chance of long-term remission, or even cure, but can incur life-threatening side effects.
The treatment for AML is intense and can be traumatic. Patients are generally required to remain in hospital for extended periods of time, and often undergo multiple rounds of chemotherapy. Side effects will vary depending on the type of treatment the patient has, but often include anemia, nausea, fatigue, diarrhea, hair loss, mouth ulcers and bleeding. Most AML treatments also cause infertility.
Even after the grueling ordeal of AML treatment, survival rates from AML are one of the lowest for all forms of cancer – with an estimated survival rate of just 13.6% after 5 years.
KR: Can you explain the research focus of Dr. Kevin Rattigan and the potential impact on AML treatment?
KN: Through previous research, Dr. Rattigan has uncovered a checklist of nutrients that AML needs to survive. Some of these might not be essential for normal cells in our bodies but are crucial for AML cells. Dr. Rattigan has now developed a protein that can lower the levels of one of these key nutrients.
As part of his John Goldman Fellowship, Dr. Rattigan now wants to test if his developed protein works in experiments that mimic what might happen in real patients. His research will test if this protein could be a potential new treatment option to slow or stop leukemia and, if so, whether it could be combined with existing AML treatments to make them more effective.
Dr. Rattigan also wants to make sure that this potential new treatment only affects leukemia cells and not normal cells of the body. This would help to drastically reduce the potential side effects of AML treatment.
KR: What is the role of MYB in AML cells, and how does Dr. Noelia Che's research on the MYB protein aim to improve the treatment outcomes for AML patients?
KN: MYB is a protein that plays a crucial role in the survival of AML. One role appears to include controlling how leukemia cells use glucose – their primary source of energy. Despite the clear importance of MYB in AML, the protein has so far been deemed “undruggable”, as finding ways to target it remain elusive.
Dr. Che and her team have already discovered that MYB relies on a specific enzyme that plays a key role in glucose breakdown and could be important for survival. During her John Goldman Fellowship, Dr. Che will investigate whether targeting this enzyme could be a way of stopping AML in its tracks.
The ultimate goal of Dr. Che’s research is to find ways to interrupt AML’s ability to use glucose efficiently, which could lead to the development of better, more precise treatment options.
This research could offer hope to those AML patients who currently have limited treatment options or who don’t respond well to existing therapies.
KR: What is the significance of Dr. Simona Valletta's investigation into the CCR1 protein and its effect on leukemia progression?
KN: Dr. Valletta and her team are interested in the environment that surrounds leukemia cells – the microenvironment. The team want to understand how the microenvironment acts to protect AML cells, by supporting cell growth and resistance to therapy. They are particularly interested in the role of a protein called CCR1, which they previously found to be highly expressed in both mice and humans with AML.
During her John Goldman Fellowship, Dr. Valletta will investigate the role of CCR1 in detail. She will use a molecule capable of blocking this protein to work out whether this affects leukemia progression and the surrounding microenvironment. Dr. Valletta will use new technology to study each individual microenvironment cell and determine which are most harmful. The same approach will be used to investigate if these harmful cells in the environment change when CCR1 is blocked, providing less support to leukemia and halting progression of the disease.
Targeting CCR1 to exploit the microenvironment in AML has the potential to significantly improve AML treatment in the future. This strategy could be used to complement existing treatments, as well as helping to overcome treatment resistance.
KR: Can you surmise Dr. Sophie Kellaway's research into how mutations in RUNX1 cause AML?
KN: One type of AML, which makes up 1 in 10 cases, is caused by a mutation in a gene called RUNX1.
The product of the RUNX1 gene is central in coordinating how blood cells are made. There are nearly 100 different mutations in RUNX1 which cause AML, but we don’t know if these mutations all have the same effect, as response to treatment can vary.
During her John Goldman Fellowship, Dr. Kellaway will investigate how different types of RUNX1 mutation cause the instructions for making blood cells to go wrong and how this leads to AML.
The project will assess the role of each of these mutations in detail – highlighting similarities and differences and mapping out how they influence the development of AML. It’s hoped that expanding understanding about the many different RUNX1 mutations will ultimately help doctors decide which of the currently available treatments will work best for each patient.
Kate Nash was speaking to Kate Robinson, Assistant Editor for Technology Networks.